How to Integrate Dissociation Into EMDR Case Conceptualization: A Practical Guide for Trauma Therapists
Feb 13, 2026
Written By: The
Read Time: 9 Minutes
Why Dissociation Needs Its Own Case Map
You've completed EMDR basic training. You know the AIP model, can identify targets, and run the protocol. But then you meet Elena.
Elena dissociates frequently. She loses time between appointments. She describes herself in fragments: "the work version," "the angry one," "the little girl who hides." When you ask about trauma, different parts hold different pieces, and they don't all agree EMDR is safe.
Your training didn't prepare you for this. You're stuck between proceeding with standard EMDR (risky) and avoiding trauma processing (unhelpful). So you hesitate.
Here's the problem: most EMDR and trauma clinicians were never given integrated training on dissociation. We learned the eight phases and bilateral stimulation, but not how to map dissociative systems or adapt protocols when consciousness itself is fragmented.
Dissociation is common across the trauma spectrum, not just in DID. It shows up in complex PTSD, attachment trauma, and developmental trauma. Ethical practice requires "assessment before activation" mapping the dissociative landscape before processing, not pushing ahead with standard protocols.
This article shows you how to integrate dissociation into EMDR case conceptualization using the AIP model you already know.
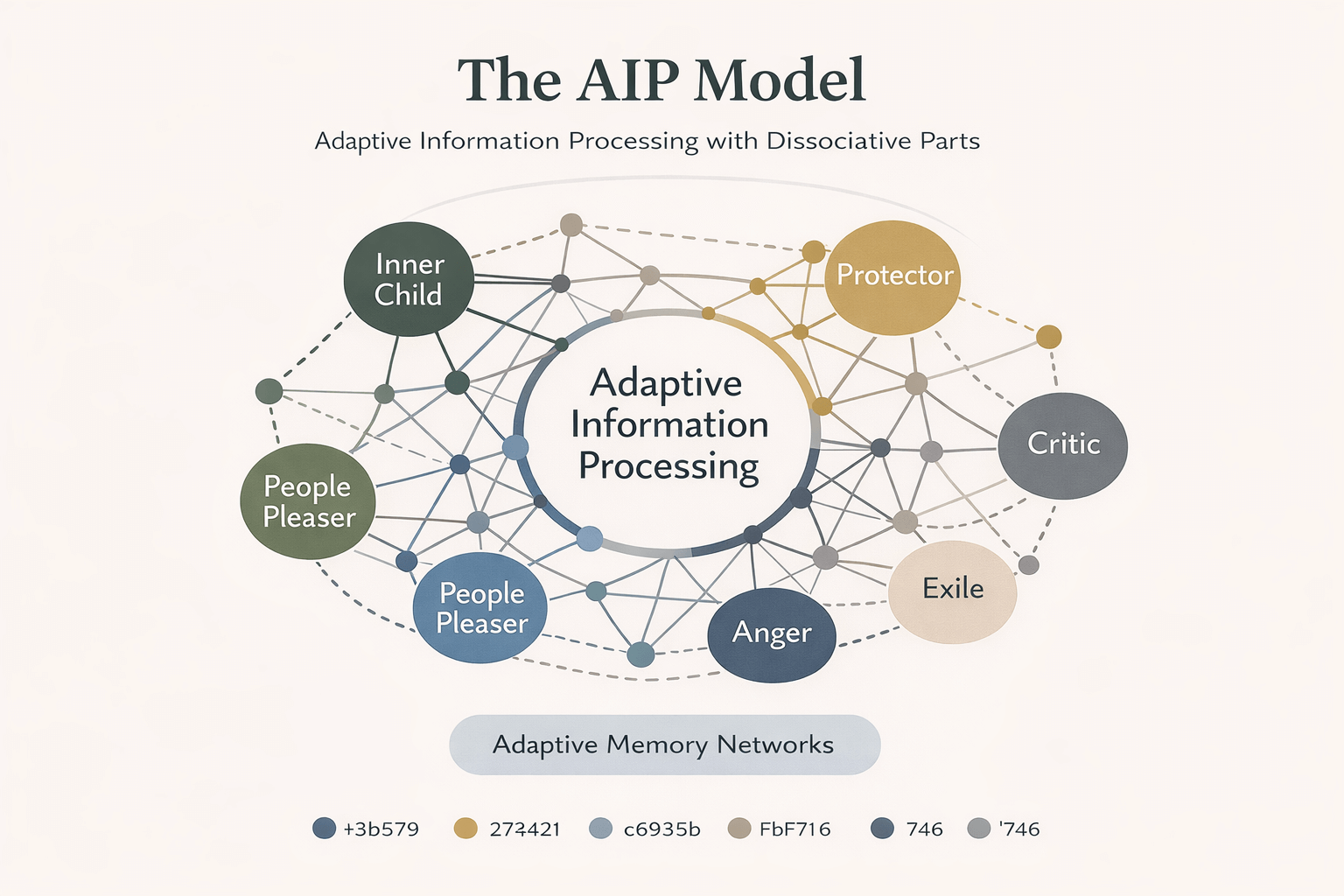
Folding Dissociation Into the AIP Model
You already know AIP: trauma happens when disturbing experiences get stored dysfunctionally, fragmented, stuck in neural networks with original emotions, body sensations, and beliefs intact. EMDR works by activating those networks and allowing natural integration.
Now add dissociation.
Dissociative parts are networks of unprocessed, state-dependent memory, belief, affect, and sensation. The fragmentation isn't just about individual memories, it's about different self-states holding different trauma networks, beliefs, resources, and relationships to the present.
In standard work, you're helping one person integrate fragmented memories. In dissociation-informed work, you're helping a system of parts integrate both their trauma networks and their relationships to each other.
Here are dissociation-aware AIP formulations:
Attachment-based: "When attachment threat activates, the 'protector' part takes over with rage and substance use to block contact with younger, terror-held networks. The adult part has resources but can't access them when protector is activated."
Shame-based: "The competent work self holds no trauma and believes 'I'm capable.' The younger part holds abuse memories and believes 'I'm disgusting.' They operate in separate networks, creating identity confusion when triggers activate the shame network."
Survival switching: "When reminded of neglect, the client shifts into dissociative numbing and cognitive fog (freeze response). This state holds the implicit memory 'showing feelings means abandonment,' blocking current relational resources."
These position dissociative parts within AIP, not outside it. Parts are trauma networks organized by state-dependency, operating by the same information processing principles you understand.
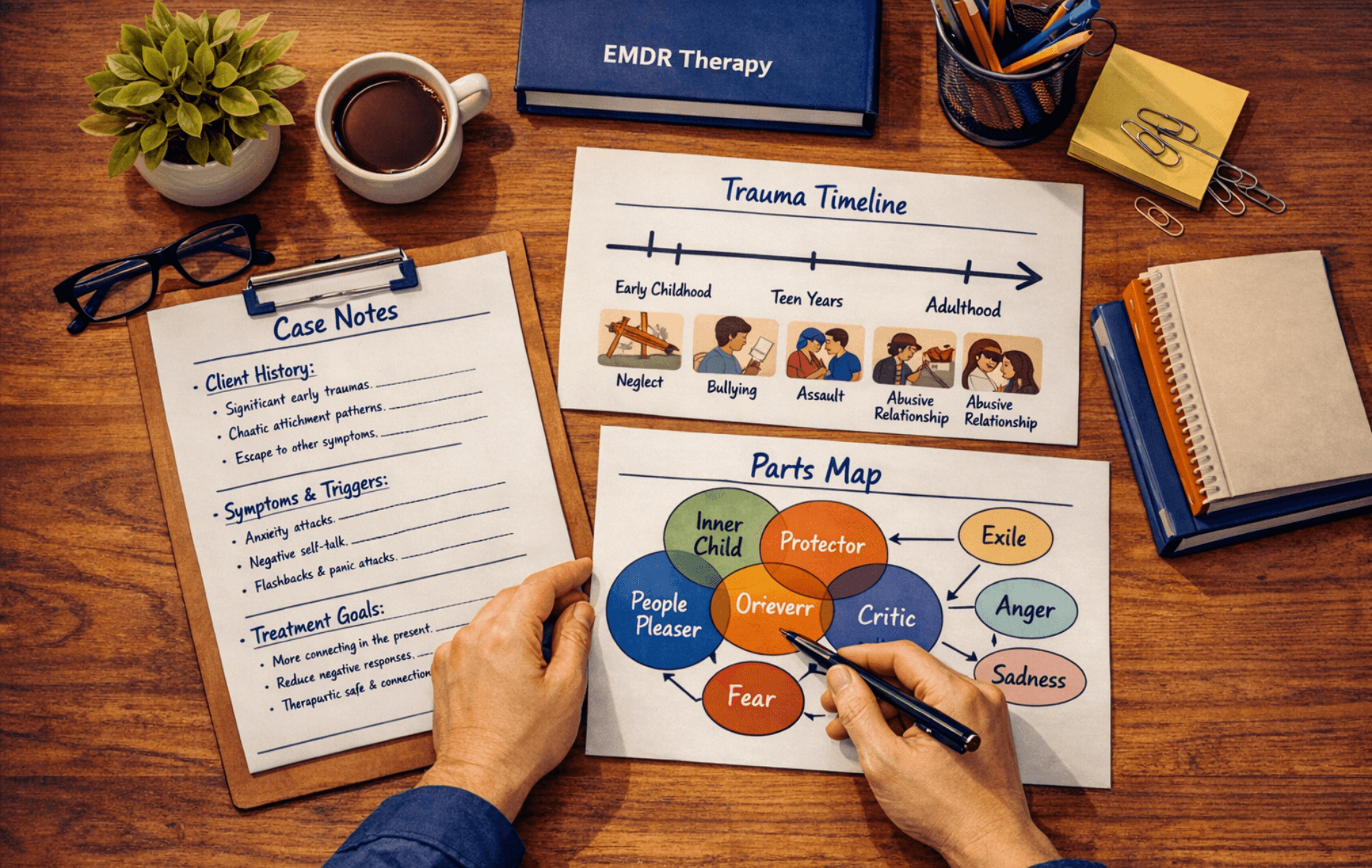
Practical Steps in Dissociation-Informed Case Conceptualization
Here's a repeatable process:
Step 1: Clarify Presenting Problems and Dissociative Symptoms
Assess standard presenting concerns plus dissociative clusters:
Time loss/amnesia: "Do you lose chunks of time?" "Found evidence of things you did but don't remember?"
Identity disturbance/parts: "Feel like different versions of yourself?" "Ever feel like a completely different person?"
Emotional numbing: "Feel like you're watching life from outside your body?" "Times when you can't feel anything?"
Depersonalization/derealization: "Does the world feel unreal?" "Feel disconnected from your body or thoughts?"
Listen for phenomenology, how clients describe experiences in their words.
Step 2: Map Parts Using Client Language
Create a map of the internal system using whatever language clients use parts, versions, identities, modes.
- Which parts exist
- What each holds (memories, beliefs, emotions, protective functions)
- How they relate (cooperative, conflicted, unaware)
- Which show up in daily life vs only under stress
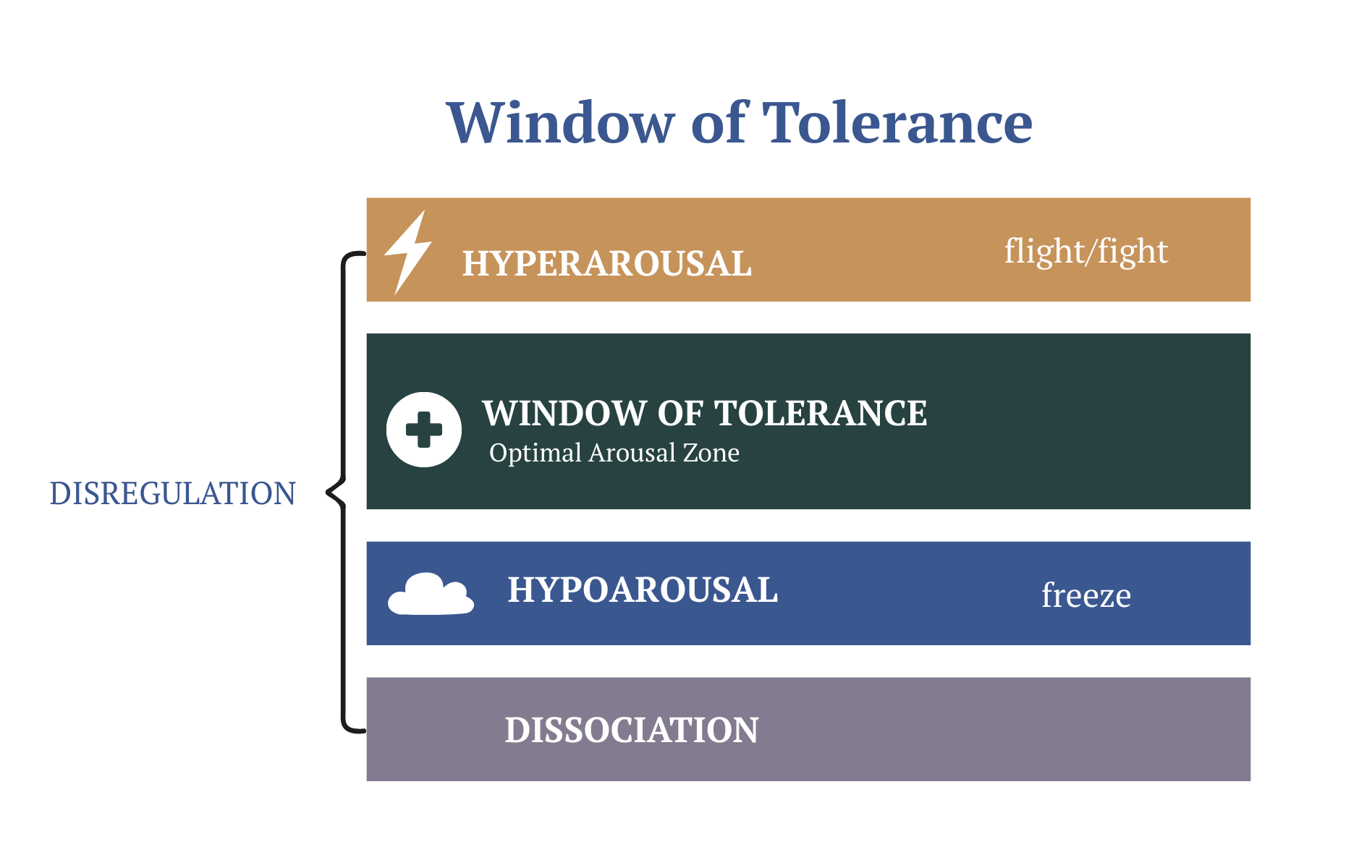
Place this in a Window of Tolerance frame. Which parts operate in the window? Which live above (hyperaroused) or below (hypoaroused)?
Step 3: Distinguish Adaptive vs Maladaptive Dissociation
When does dissociation serve the person vs interfere with life?
Look for:
- Functional impairment (work, relationships, safety)
- Distress level
- Interference with goals
Identify safety and risk indicators. Which parts are stable? Volatile? Self-destructive? Internal conflicts that could escalate?
Step 4: Create a Dissociative Profile
A dissociative profile answers:
- System structure (parts, states, amnesia degree)
- Which parts hold which trauma
- Which have resources vs complete dysregulation
- Internal agreements/conflicts about trauma work
- High-risk areas (suicidality, self-harm, substances)
This profile directly informs EMDR readiness, resource building, and target selection.
What Changes in EMDR Target Selection and Pacing
Standard EMDR target selection often follows a "top ten worst memories" approach. You ask about the most disturbing events, create a timeline, and start processing based on clinical judgment about which memory is most central.
With dissociative clients, that approach can be dangerous.
Target Selection Shifts
Instead of "worst memories first," you're asking: "Which targets is the system willing and resourced to approach?"
This requires collaboration with protective parts. Before you target anything, you're checking:
- Does the part that holds this memory feel ready to work on it?
- Are protective parts on board, or will they shut things down mid-session?
- Do we have enough internal communication for the system to handle what comes up?
- Is there agreement across parts that this target serves everyone's goals?
Sometimes the "worst" trauma isn't accessible yet because protective parts are blocking it for good reason. So you might start with:
- Current triggers that activate dissociative responses
- "Bridge" memories that multiple parts have access to
- Preparation targets that build system cohesion (positive memories, resource states)
- Smaller trauma memories that test the system's capacity before going deeper
The goal is building trust and demonstrating that EMDR can work safely for this particular system, not forcing access to material they're not ready to process.
Pacing Changes
Pacing shifts dramatically with dissociative presentations:
More time in Phases 1 and 2. You're not rushing to reprocessing. You're spending weeks or months mapping the system, building resources across parts, establishing internal communication, and creating safety agreements. This isn't "just doing stabilization." It's essential for assessment and preparation.
Modified bilateral stimulation for dual awareness. Some dissociative clients need slower BLS, shorter sets, or different types of stimulation to maintain dual awareness (awareness of both the past trauma and present safety). When clients drift too far out of the window, you're adjusting in real time.
Phase-specific adjustments to prevent flooding. You're watching for dissociative drift during processing, the glazed look, the time distortion, the sudden flatness. When you see it, you're slowing down, checking in more frequently, and possibly pausing processing altogether if a part is getting overwhelmed.
The mantra is: competence includes pacing. Going faster doesn't make you a better EMDR therapist. Going at the pace the system can handle does.
Brief Case Vignettes and Sample Formulations
Let's make this practical with real examples.
Vignette 1: Sarah, 38, Complex PTSD with Parts
Presentation: Sarah came in for "anxiety and relationship problems." In assessment, she described three distinct self-states: Adult Sarah (competent, works in tech), Young Sarah (holds abuse memories, age 7), and Protector (angry, suspicious, blocks access to Young Sarah).
Standard approach would have been: Target the abuse memories directly, probably starting with "the worst one."
Dissociation-informed case map revealed: Young Sarah holds the trauma networks, but Protector shuts down any attempt to access them. Adult Sarah has resources but can't reach Young Sarah when Protector is activated.
AIP formulation: "When attachment needs surface (current trigger), Protector activates with rage and withdrawal (adaptive protection strategy) to prevent Young Sarah's terror from flooding the system (unprocessed trauma network). Adult Sarah's resources are blocked by parts conflict."
Dissociation plan: "Build resources for Protector first (anger management, boundary skills). Facilitate communication between Adult Sarah and Protector. Only approach Young Sarah's trauma when the Protector agrees it's safe."
EMDR implementation: Spent 8 weeks in Phase 2 doing parts mapping and internal negotiation. First EMDR target was actually a positive memory where Protector successfully kept Sarah safe, strengthening Protector's trust in the process. Only then moved to abuse memories, with Protector's explicit permission.
Result: Processing happened without destabilization because the system was prepared and collaborative.
Vignette 2: Marcus, 45, Dissociative Responses in Addiction Treatment
Presentation: Marcus in residential treatment for alcohol use. Described "watching himself drink" and time loss around use. Has a "sober self" who commits to recovery and a "using self" who takes over during stress.
Standard approach: Focus on relapse triggers and addiction timeline.
Dissociation-informed case map: The "using self" is actually a dissociative state that activates under stress, holds unprocessed trauma from childhood neglect, and uses alcohol to stay numb. The "sober self" has no access to those trauma networks.
AIP formulation: "When abandonment fear activates (current trigger), the using state takes over with dissociative numbing and alcohol use (adaptive escape from unbearable affect) to block access to childhood neglect memories (unprocessed trauma). Sober self and using self operate in separate networks."
Dissociation plan: "Map both states. Build resources in sober state. Facilitate communication between states. Target neglect memories only when both states agree and using state has alternative coping besides substances."
EMDR implementation: Used slower BLS (4-6 passes instead of 24+) when processing activated the using state. Checked in every set: "Which part is here right now? What do you need?" Built containment skills specifically for the using state.
Result: Could stay in window of tolerance during processing. Sober state and using state began communicating, reducing sudden switches.
Vignette 3: Jen, 29, DID with High Parts Conflict
Presentation: Diagnosed DID, seven distinct parts with significant amnesia between them. Parts don't agree on therapy goals. Some want integration, others want to maintain separation.
Standard approach: This case would likely get referred out as "too complex."
Dissociation-informed case map: Identified which parts held which trauma networks. Discovered that parts conflict was actually about different survival strategies (submission vs fighting vs fleeing) that hadn't been integrated.
AIP formulation: "Different parts developed around incompatible survival responses to chronic abuse (freeze, fight, flee). Each part holds networks associated with their survival role. Conflict arises when current situations activate multiple parts with different strategies."
Dissociation plan: "Work with parts as a system, not individually. Build co-consciousness between parts. Target trauma memories only when there's internal agreement. Goal is cooperation, not forced integration."
EMDR implementation: Did EMDR with "the system" present, not just one part. Used interweaves like "What does each part need right now?" Modified closure to ensure all parts felt contained before ending session.
Result: Parts conflict decreased significantly. Could process trauma collaboratively rather than against internal resistance.
When to Seek Dissociation-Specific Training
How do you know when you're in over your head and need specialized dissociation therapist training?
Watch for these red flags:
Repeated looping during processing. The client processes the same material over and over with no decrease in disturbance. This often means a protective part is blocking integration.
Uncontrolled switching between parts. The client shifts rapidly between states during the session and you can't track what's happening or help them ground.
Extended time loss in or after sessions. The client loses significant chunks of time around EMDR work, suggesting the processing is flooding the system.
Your own fear or confusion. If you're consistently anxious about sessions, avoiding certain topics, or feeling lost about what to do next, that's clinical information. It likely means you need more training.
Parts conflict escalating. Internal fighting gets worse during trauma work instead of better, or self-harm/suicidality increases.
Client feedback that something's wrong. They tell you EMDR makes things worse, or certain parts are angry about the treatment approach.
These aren't signs of clinical failure. They're signs you need additional competencies that basic EMDR training doesn't provide.
Where to Get Dissociation-Specific EMDR Training
The Clinical Competencies in Treating Dissociative Identities training is specifically designed for this gap. It's structured, competency-based dissociation EMDR therapist training for USA-based clinicians who need practical skills, not just theory.
The focus is exactly what you need:
- Assessment before activation: How to map dissociative systems before processing
- Pacing across all eight phases: When to go slower, how to modify BLS, what interweaves work with parts
- Phase-specific EMDR adaptations: Not just general dissociation knowledge, but concrete protocol modifications
This isn't about becoming a dissociation specialist. It's about building core competencies so you can work ethically and effectively with the dissociative presentations already in your caseload.
Frequently Asked Questions
How do I know if I need dissociation-specific EMDR therapist training?
If you regularly encounter clients who lose time, describe parts or different self-states, show rapid shifts in affect or presentation, or seem to "go away" during processing, you need dissociation training. If you're avoiding EMDR with certain clients because you're worried about destabilization, or if your standard protocols aren't working with complex presentations, that's a clear signal. Formal dissociation training teaches assessment, case conceptualization, and adaptation skills that basic EMDR certification doesn't cover.
How does dissociation change EMDR case conceptualization and target selection?
Dissociation requires mapping the internal system of parts or states before targeting trauma. Instead of selecting targets based solely on "worst memories," you're asking which targets the system is willing and able to approach. You're collaborating with protective parts, checking for internal agreement, and choosing targets based on system readiness rather than just clinical logic. Case conceptualization becomes about understanding which parts hold which trauma networks, how they relate to each other, and what preparation is needed before processing.
What practical adjustments should EMDR therapists make when working with dissociative clients?
Key adjustments include: spending more time in Phases 1 and 2 for thorough assessment and preparation; using modified bilateral stimulation (slower, shorter sets) to maintain dual awareness; checking in more frequently during processing to track which part is present; employing parts-specific interweaves; implementing robust closure protocols that address all parts; and pacing treatment based on system capacity rather than clinical timelines. The foundational shift is moving from standard protocols to dissociation-adapted protocols that prioritize safety and system collaboration.
Building Your Dissociation Competencies
Here's what you need to take away: dissociation doesn't invalidate the AIP model you already know. It deepens it.
When you understand dissociative parts as state-dependent trauma networks, you can use your existing EMDR framework. You're just applying it to a system of parts instead of a single unified consciousness. The principles stay the same. The adaptations are learnable.
The clients are already in your office. The ones who lose time, switch between states, hold trauma in fragments, and need more than standard protocols. They're not "too complex" for EMDR. They need dissociation-informed EMDR from therapists who have the training to provide it safely and effectively.
If you're ready to move from hesitation to competence, from avoiding complexity to working skillfully within it, specialized training is your next step. Learn how to map dissociative systems, select targets collaboratively, pace treatment appropriately, and adapt all eight phases for clients whose consciousness is fragmented.
Because the field needs trauma therapists who can handle complexity. And your clients deserve clinicians who see dissociation not as a barrier to treatment but as essential information about how their trauma got stored and how it can finally be processed.
Ready to build dissociation competencies for your EMDR practice? The Clinical Competencies in Treating Dissociative Identities training offers structured, practical guidance on case conceptualization, assessment, and phase-specific adaptations. Join EMDR and trauma therapists across the USA building these essential skills. Registration is open now.
References
Ad De Jongh, Laurian Hafkemeijer, Hofman, S., Slotema, K., & Hornsveld, H. (2024). The AIP model as a theoretical framework for the treatment of personality disorders with EMDR therapy. Frontiers in Psychiatry, 15. https://doi.org/10.3389/fpsyt.2024.1331876
Advanced Certificate in Dissociation Studies for EMDR Therapists. (2021, December 14). The Institute for Creative Mindfulness. https://www.instituteforcreativemindfulness.com/advanced-certificate-in-dissociation/
Clinical Competencies in Treating Dissociative Identities. (2019). Traumatherapistinstitute.com. https://www.traumatherapistinstitute.com/Clinical-Competencies-in-Treating-Dissociative-Identities-Bridging-Lived-Experience-and-Science-For-the-Trauma-Therapist
Dissociation and EMDR | EMDR therapy. (2025). Teachable.com. https://therapisteducationinstitute.teachable.com/p/dissociation-and-emdr
Dissociative Identity Disorder in Clinical Practice: A Trauma-Informed Guide for Mental Health Professionals. (2025, October 22). Leading Edge Seminars. https://leadingedgeseminars.org/event/dissociative-identity-disorder-in-clinical-practice-webinar/
EMDR International Association. (2024, July 24). AIP model-based acute trauma and ongoing traumatic stress theoretical conceptualization (Iberoamerican Journal of Psychotraumatology and Dissociation). EMDR International Association. https://www.emdria.org/resource/aip-model-based-acute-trauma-and-ongoing-traumatic-stress-theoretical-conceptualization-iberoamerican-journal-of-psychotraumatology-and-dissociation/
EMDR Therapy Training - ISSTD. (2025, May 30). ISSTD. https://www.isst-d.org/training-and-conferences/training-courses/emdr-therapy-training/
Introduction to Dissociation. (2025, May 23). Blue Knot Foundation. https://professionals.blueknot.org.au/professional-development-training/training-programs/introduction-to-dissociation/
Stay connected with fun info, news, promotions and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.